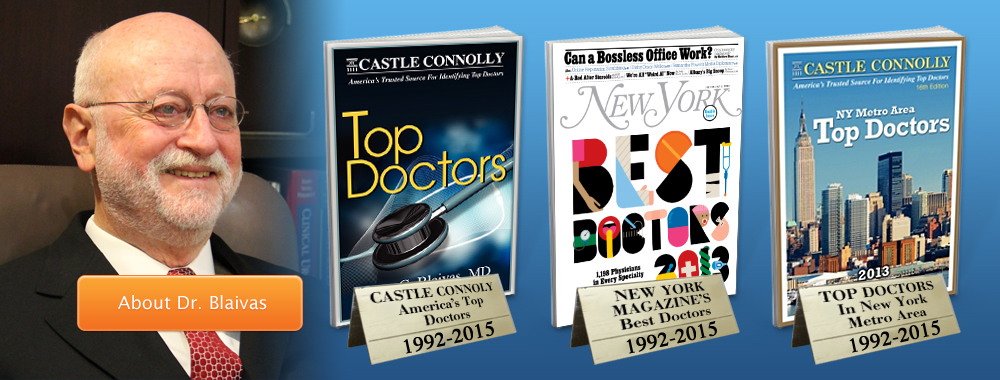
Jerry G. Blaivas, MD, FACS
Dr. Blaivas is a world-renowned urological expert, surgeon, distinguished author, educator, and medical pioneer. He was one of the founders of urodynamics and established many of the current surgical procedures used to correct stress incontinence, urinary fistulas, urethral diverticulum, overactive bladder and neurogenic bladder.
He is also one of the few surgeons who routinely performs reconstructive surgery for prolapse and incontinence without the use of mesh. His success in this area has led him to publishing one of the largest series in the world on treatment of mesh complications.
Dr. Blaivas possesses decades of experience providing urology care to some of the most complex cases ever encountered, bringing academic and research-based modernization to the clinical forefront. His research in developing new medical techniques has become the standard in patient care, including breakthrough treatments and research in:
- Mesh complications
- Radiation complications
- Autologous Slings
- Natural Tissue Repairs
Dr. Blaivas was recently honored by the Canadian Journal of Urology as one of their Legends of Urology. Read the article >
Schedule an appointment online or call Dr. Blaivas today at (646) 205-3039 to schedule a confidential consultation.
Insurance Information
Dr. Blaivas does not participate with private insurance plans. He is considered an “Out of Network” physician, which means that payment in full is expected at the time of the visit and you will be reimbursed directly according to your insurance plan. As a courtesy, we offer to complete and mail claims on your behalf and assist you in obtaining timely reimbursement.
About the Uro Center of New York
At the Uro Center of New York, we combine clinical and academic excellence in a private practice setting. For over twenty years, our staff has been committed to diagnosing and treating people with bladder and prostate conditions. Our services include the use of state-of-the-art video urodynamic equipment and a custom-designed computer system that assists our physicians in ensuring an accurate and prompt diagnosis.




 Bladder cancer is one of the most common forms of cancer. Statistically, it affects men more than women. Adults are more at risk to be affected, but it can happen at any point in life. Almost 7 out of 10 times, bladder cancer is detected in patients at an early stage. It is the point when it is highly treatable. At the same time, patients who have undergone treatment for bladder cancer successfully, need to follow up tests for years as it has a high probability to recur.
Bladder cancer is one of the most common forms of cancer. Statistically, it affects men more than women. Adults are more at risk to be affected, but it can happen at any point in life. Almost 7 out of 10 times, bladder cancer is detected in patients at an early stage. It is the point when it is highly treatable. At the same time, patients who have undergone treatment for bladder cancer successfully, need to follow up tests for years as it has a high probability to recur. Some of the common symptoms of Bladder Cancer are:
Some of the common symptoms of Bladder Cancer are:
 A cystocele is a medical condition that is also referred to as dropped, prolapsed, or fallen bladder. This occurs in women when the bladder either drops or expands into the vagina. A cystocele can lead to uncomfortable urination. There are three levels of cystoceles. Grade One is mild, and means that the bladder is only partially in the vagina. In Grade Two, which is more severe, the bladder is far enough in the vagina that it has reached the outside of the vagina. The most advanced stage, Grade Three, means that the bladder has moved through the vagina, which connects the uterus to the outside of the body.
A cystocele is a medical condition that is also referred to as dropped, prolapsed, or fallen bladder. This occurs in women when the bladder either drops or expands into the vagina. A cystocele can lead to uncomfortable urination. There are three levels of cystoceles. Grade One is mild, and means that the bladder is only partially in the vagina. In Grade Two, which is more severe, the bladder is far enough in the vagina that it has reached the outside of the vagina. The most advanced stage, Grade Three, means that the bladder has moved through the vagina, which connects the uterus to the outside of the body. There are several causes of cystocele. One of these causes is muscle strain while giving birth. Heavy lifting, being overweight or obese, or regular difficult bowel movements can also cause strain on the muscles of the bowel, which can lead to a cystocele. A cystocele can also develop during menopause because women stop producing estrogen. Since estrogen is one of the things that keeps the muscles in the vagina strong, when the body is no longer producing estrogen the muscles may become weaker. This can lead to a cystocele, though there is some debate as to whether or not menopause causes a cystocele.
There are several causes of cystocele. One of these causes is muscle strain while giving birth. Heavy lifting, being overweight or obese, or regular difficult bowel movements can also cause strain on the muscles of the bowel, which can lead to a cystocele. A cystocele can also develop during menopause because women stop producing estrogen. Since estrogen is one of the things that keeps the muscles in the vagina strong, when the body is no longer producing estrogen the muscles may become weaker. This can lead to a cystocele, though there is some debate as to whether or not menopause causes a cystocele. The treatment for cystocele can be different, depending on the grade of the cystocele and how long it’s been there. One treatment for a cystocele is a surgery that will put the bladder and urethra back into the position that they are supposed to be in. After surgery, it is recommended that patients avoid standing for a long time or heavy lifting. Although they can gradually go back to their normal activities, too much strain can render the surgery useless. Other treatment options include avoiding straining those muscles, a series of exercises, and an implant to hold the bladder in place.
The treatment for cystocele can be different, depending on the grade of the cystocele and how long it’s been there. One treatment for a cystocele is a surgery that will put the bladder and urethra back into the position that they are supposed to be in. After surgery, it is recommended that patients avoid standing for a long time or heavy lifting. Although they can gradually go back to their normal activities, too much strain can render the surgery useless. Other treatment options include avoiding straining those muscles, a series of exercises, and an implant to hold the bladder in place. Urologic Problems in Men
Urologic Problems in Men Urologic Problems in Women
Urologic Problems in Women